Contents
- Healthcare Infrastructure
- The Three-Tiered Structure in the District
- Post-Independence Growth: 1950-1961
- Medical Education & Research
- Government Medical College
- ICMR Centre for Research, Management and Control of Haemoglobinopathies
- Age Old Practices & Remedies
- Home Remedies and Local Knowledge
- Ayurvedic Medicine and Commercial Preparations
- Local Beliefs Related to Illness
- Evolution of Public Health Service in the District
- Disease Control Initiatives: 1948-1958
- Contemporary Challenges: Water Management & Healthcare Accessibility
- COVID-19 in Chandrapur
- Dr. Ramchandra Danekar
- Graphs
- Healthcare Facilities and Services
- A. Public and Govt-Aided Medical Facilities
- B. Private Healthcare Facilities
- C. Approved vs Working Anganwadi
- D. Anganwadi Building Types
- E. Anganwadi Workers
- F. Patients in In-Patients Department
- G. Patients in Outpatients Department
- H. Outpatient-to-Inpatient Ratio
- I. Patients Treated in Public Facilities
- J. Operations Conducted
- K. Hysterectomies Performed
- L. Share of Households with Access to Health Amenities
- Morbidity and Mortality
- A. Reported Deaths
- B. Cause of Death
- C. Reported Child and Infant Deaths
- D. Reported Infant Deaths
- E. Select Causes of Infant Death
- F. Number of Children Diseased
- G. Population with High Blood Sugar
- H. Population with Very High Blood Sugar
- I. Population with Mildly Elevated Blood Pressure
- J. Population with Moderately or Severely High Hypertension
- K. Women Examined for Cancer
- L. Alcohol and Tobacco Consumption
- Maternal and Newborn Health
- A. Reported Deliveries
- B. Institutional Births: Public vs Private
- C. Home Births: Skilled vs Non-Skilled Attendants
- D. Live Birth Rate
- E. Still Birth Rate
- F. Maternal Deaths
- G. Registered Births
- H. C-section Deliveries: Public vs Private
- I. Institutional Deliveries through C-Section
- J. Deliveries through C-Section: Public vs Private Facilities
- K. Reported Abortions
- L. Medical Terminations of Pregnancy: Public vs Private
- M. MTPs in Public Institutions before and after 12 Weeks
- N. Average Out of Pocket Expenditure per Delivery in Public Health Facilities
- O. Registrations for Antenatal Care
- P. Antenatal Care Registrations Done in First Trimester
- Q. Iron Folic Acid Consumption Among Pregnant Women
- R. Access to Postnatal Care from Health Personnel Within 2 Days of Delivery
- S. Children Breastfed within One Hour of Birth
- T. Children (6-23 months) Receiving an Adequate Diet
- U. Sex Ratio at Birth
- V. Births Registered with Civil Authority
- W. Institutional Deliveries through C-section
- X. C-section Deliveries: Public vs Private
- Family Planning
- A. Population Using Family Planning Methods
- B. Usage Rate of Select Family Planning Methods
- C. Sterilizations Conducted (Public vs Private Facilities)
- D. Vasectomies
- E. Tubectomies
- F. Contraceptives Distributed
- G. IUD Insertions: Public vs Private
- H. Female Sterilization Rate
- I. Women’s Unmet Need for Family Planning
- J. Fertile Couples in Family Welfare Programs
- K. Family Welfare Centers
- L. Progress of Family Welfare Programs
- Immunization
- A. Vaccinations under the Maternal and Childcare Program
- B. Infants Given the Oral Polio Vaccine
- C. Infants Given the Bacillus Calmette Guerin (BCG) Vaccine
- D. Infants Given Hepatitis Vaccine (Birth Dose)
- E. Infants Given the Pentavalent Vaccines
- F. Infants Given the Measles or Measles Rubella Vaccines
- G. Infants Given the Rotavirus Vaccines
- H. Fully Immunized Children
- I. Adverse Effects of Immunization
- J. Percentage of Children Fully Immunized
- K. Vaccination Rate (Children Aged 12 to 23 months)
- L. Children Primarily Vaccinated in (Public vs Private Health Facilities)
- Nutrition
- A. Children with Nutritional Deficits or Excess
- B. Population Overweight or Obese
- C. Population with Low BMI
- D. Prevalence of Anaemia
- E. Moderately Anaemic Women
- F. Women with Severe Anaemia being Treated at an Institution
- G. Malnourishment Among Infants in Anganwadis
- Sources
CHANDRAPUR
Health
Last updated on 6 November 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.
The healthcare landscape of Chandrapur district, like many other regions in India, is shaped by pluralistic health traditions. Folk medical traditions, biomedicine, and other medical systems each play a vital role in addressing the diverse health needs of the local community. The district’s healthcare infrastructure has been historically influenced by its distinct topographical features. Alex George and Sunil Nandraj, in their paper State of Health Care in Maharashtra: A Comparative Analysis (1993), mention that Chandrapur is among the few regions in Maharashtra that hold a “higher percentage of land area under forests” and where “scheduled tribes are (more) concentrated.”
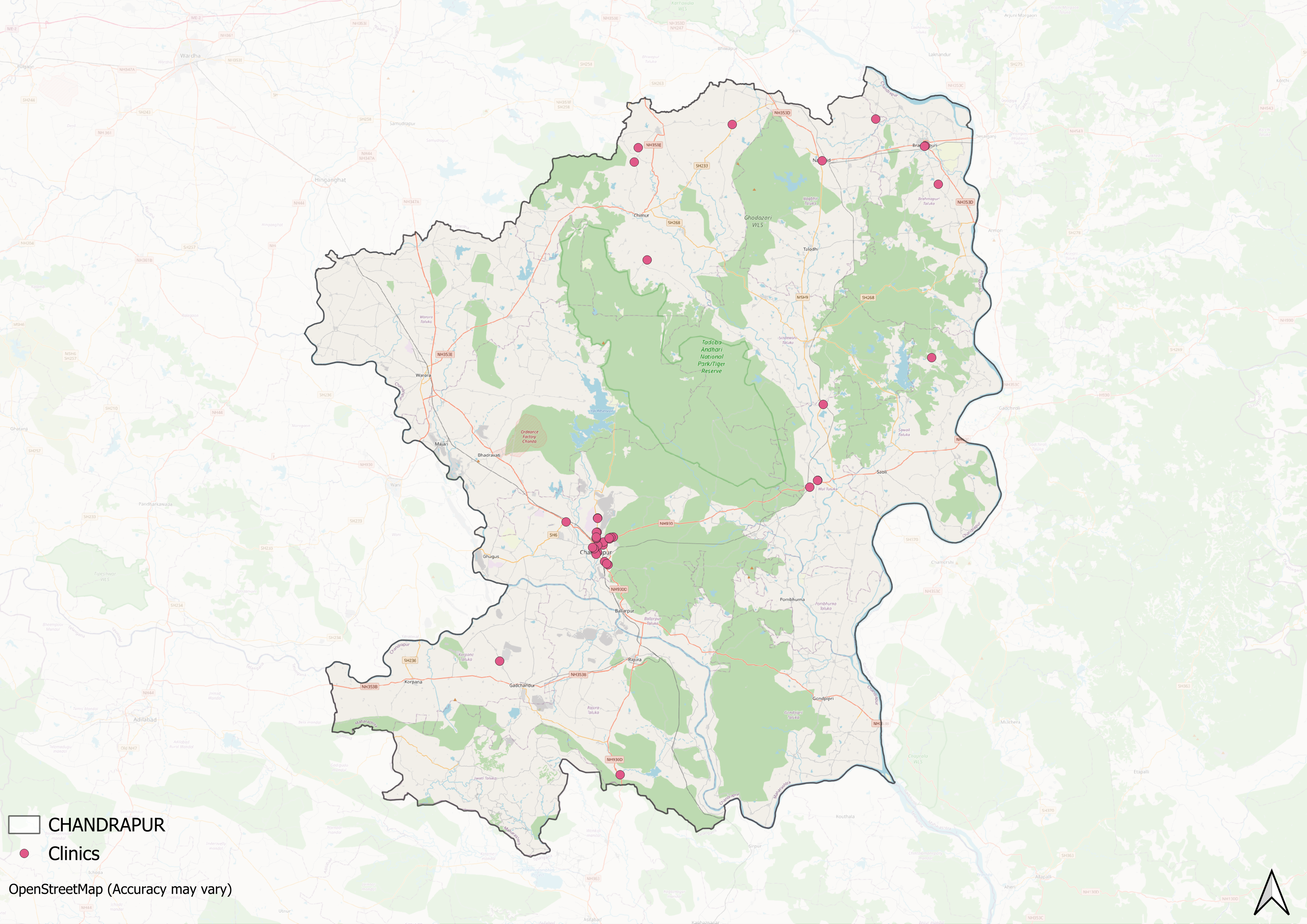
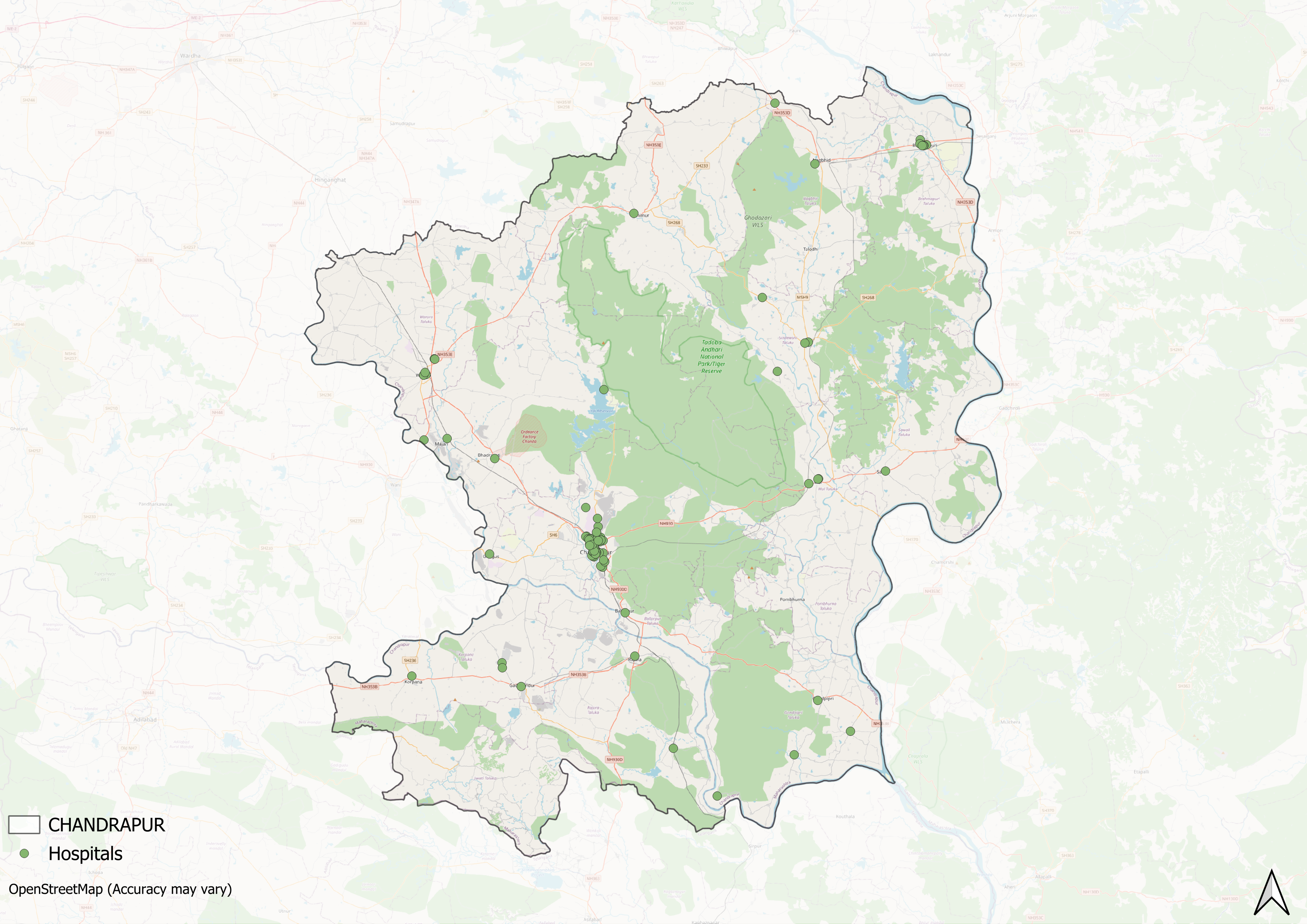
Its geographical features and dispersed communities pose persistent challenges for equitable healthcare access. The 2019 Minutes of Meeting (MoM) for the State’s Water Plan highlights this disparity, identifying Chandrapur among regions with underserved public healthcare facilities. Over the years, private healthcare providers, driven by local medical professionals, have emerged to address these gaps, though their efforts remain largely concentrated in Chandrapur taluka. While such institutional developments are significant, the district’s healthcare system also draws particular strength from dedicated individuals working across remote areas. The commitment of its healthcare workers is evident in stories like that of an 87-year-old homeopathic doctor who travels across villages to provide care; his work illustrates both the perseverance and ongoing gaps that characterize the district's healthcare landscape.
Healthcare Infrastructure
Much like other regions in India, Chandrapur’s healthcare infrastructure follows a multi-tiered system that involves both public and private sectors. Currently, the public healthcare system is tiered into primary, secondary, and tertiary levels. Primary care is provided through Sub Centres and Primary Health Centres (PHCs), while secondary care is managed by Community Health Centres (CHCs) and Sub-District hospitals. Tertiary care, the highest level, includes Medical Colleges and District Hospitals. This system has been shaped and refined over time, influenced by national healthcare reforms.
The Three-Tiered Structure in the District
The foundations of Chandrapur’s healthcare system trace back to the early 20th century, when the district established its first network of medical facilities. According to the district colonial gazetteer (1909), the region maintained 13 dispensaries across various locations, funded through a collaborative model involving government resources, local bodies, and private contributors.
In the colonial period, healthcare facilities were concentrated in key areas. Chandrapur taluka maintained two dispensaries, along with a police hospital and the Chanda Victoria Hospital, established in 1906 with a twelve-patient capacity. Healthcare services extended to other talukas through various facilities: Warora Dispensary accommodated five patients, Bramhapuri Dispensary served four patients, and Mul Dispensary had a capacity for one patient. Additionally, a specialized healthcare facility, the Colliery Dispensary at Ballalpur, was established to cater specifically to the healthcare needs of miners, indicating that early attention was given to occupational health in the district. Another noteworthy aspect of this early infrastructure was the provision of midwifery services at the Chanda and Warora dispensaries, highlighting the early attention given to maternal healthcare.
Data from the gazetteer suggests that the majority of the healthcare infrastructure was developed in the late 19th and early 20th centuries, with a primary focus on establishing primary care services.
Post-Independence Growth: 1950-1961
The post-independence era brought significant changes to Chandrapur’s healthcare landscape. According to the district gazetteer (1972), Chandrapur taluka operated four hospitals by 1950. During this time, Chandrapur taluka was operating four hospitals, one of which was the District General Hospital. The geographic expansion of healthcare services occurred gradually over the years, alongside a steady increase in medical staffing.
Data from the district gazetteer documents the evolution of healthcare staffing in Chandrapur taluka during the post-independence period. In 1950-51, medical personnel remained limited, with only eleven doctors and one nurse serving the entire taluka. The situation improved steadily over the following decade. By 1960-61, the medical workforce had expanded to twenty-six doctors and thirty-two nurses, reflecting growing local participation in healthcare services. During this same period, while Bramhapuri taluka maintained two hospitals and Warora taluka operated four, Warora faced continued staffing constraints with only eight doctors.
At present, Chandrapur is a large district comprising approximately fifteen talukas, and, as is often the case, generally, the growth of healthcare services has not been uniform across the region. However, public healthcare coverage has expanded significantly according to District Statistical Abstract (DSA) data from 2021. In 2021, nearly all talukas, except for Pombhurna and Jivati, were home to at least one public hospital. Notably, recently, authorities established a new hospital in Pombhurna, which has grown to become one of the district’s largest government medical facilities.
In recent years, a notable trend has been the rise of private healthcare providers. DSA data reveals a dramatic increase in private hospitals within Chandrapur taluka, growing from 13 facilities in 2012 to 102 in 2021. However, this private sector expansion remains concentrated in Chandrapur taluka, while other talukas continue to rely primarily on public health centers (PHCs) and sub-clinics for medical care.
Medical Education & Research
Medical education and research are foundational to a district’s healthcare infrastructure. As Mathew Gerge aptly highlights, medical institutions often serve a “dual purpose,” which includes educating future healthcare professionals and providing healthcare services to the local population. In Chandrapur, this link has grown gradually over the decades, supported mainly by private and government-aided institutions.
Government Medical College
Government Medical College is a public medical institution established in 2015. The college offers an MBBS program with 150 seats and maintains affiliation with the Maharashtra University of Health Sciences (MUHS), Nashik. Admissions are conducted through CET/NEET, with 85% seats allocated through state CET and 15% through All India PMT.
The institution initially operated from the premises of a TB Hospital with 100 beds, later merging with Chandrapur Civil Hospital (100 beds) and the TB Hospital run by Maharashtra's public health department.
ICMR Centre for Research, Management and Control of Haemoglobinopathies
The ICMR Centre for Research, Management, and Control of Hemoglobinopathies in Chandrapur was established by the Indian Council of Medical Research (ICMR) under the ICMR-National Institute of Immunohaematology, Mumbai. The centre is dedicated to research, training, and service related to hemoglobinopathies, including sickle cell disease and thalassemia, which are health conditions currently prioritized under the National Health Mission.
![ICMR Centre for Research, Management and Control of Haemoglobinopathies, Chandrapur.[1]](/media/statistic/images/maharashtra/chandrapur/health/icmr-centre-for-research-management-and-c_JANncsF.png)
The centre maintains comprehensive facilities including administrative offices, an auditorium, laboratory facilities, student hostel, staff housing, and guest houses. These facilities support its mission of research, training, and service delivery in hemoglobinopathy management.
The Vidarbha region, where the district is located, as per the website, hosts approximately 12,000 Sickle Cell Disease patients, with over 3,000 in Chandrapur district alone. These numbers, along with potentially undiagnosed cases, underscore the significant role that the centre likely plays in disease management and research for these conditions in the region.
Age Old Practices & Remedies
Before the establishment of Western healthcare systems and the contemporary three-tiered healthcare infrastructure, the inhabitants of Chandrapur relied heavily on indigenous knowledge and traditional medicine for their well-being. India’s healthcare paradigm has long been characterized by medical pluralism, wherein multiple healing traditions have existed in parallel, often complementing one another. In Chandrapur, as locals say, Ayurveda and folk medicine have held particular prominence. These systems, while rooted in ancient practices, have been shaped by the local geography and socio-cultural milieu; resulting in distinct regional adaptations that continue to influence the health practices of the district even today.
Home Remedies and Local Knowledge
In Chandrapur, as throughout India, traditional medical knowledge is an integral part of domestic healthcare practices. This knowledge, preserved and transmitted through generations, guides both herbal medicine and dietary practices in daily life. Local communities maintain a sophisticated understanding of medicinal plants, each valued for its specific health benefits.
Among the most commonly used plants are Khanduchakka (wild turmeric), Sabja (basil seeds), Kambarmodi (bitter gourd), Pilpila Pimpal (pepper tree), and Tulsi (holy basil). These herbs are typically prepared in the form of kadhas (herbal decoctions) or other medicinal concoctions, tailored to address specific health concerns.
In addition to everyday remedies, certain herbs are particularly effective in combating seasonal illnesses. For example, an extract prepared from two and a half leaves of Bhui Limba (Plectranthus) is traditionally used to treat persistent fever, with the preparation made just before sunrise.
Ayurvedic Medicine and Commercial Preparations
In Chandrapur, residents also frequently consult traditional healers and Ayurvedic pharmacies for many ailments. Plant-based remedies that are a major part of the Ayurvedic healing process are widely consumed. One commonly used medicine is Amrit Dhara, an oil made from mint sat, ajwain sat, and bhimseni camphor. Local residents use this preparation to treat cold, cough, fever, headache, and nausea.

Another important Ayurvedic medicine found in local pharmacies is Asli Sudha Sagar, which is sold in Shegaon, Warora Taluka. People use it to treat various conditions including cough, stomach ache, nausea, vomiting, and even bites from scorpions or snakes. It is believed that mixing a few drops of rose water with this medicine helps alleviate stomach discomfort or nausea.
Local Beliefs Related to Illness
In many communities, illness is understood not just through scientific explanations but also through cultural lenses shaped by local traditions and relationships with the environment. These local belief systems offer unique insights into how health and disease are perceived in different contexts.
In Chandrapur, a belief held by some residents pertains to typhoid. Scientifically, typhoid is caused by the bacteria Salmonella Typhi, typically spread through contaminated water or food. However, some residents of Chandrapur believe that typhoid is linked to the presence of white rot and black curly rot in trees. This interpretation diverges from the medical understanding of the transmission of the disease.
The origins of this belief are closely tied to the region’s fruit foraging traditions. Many residents forage for fruits, locally known as muris, from trees such as Umbera (Indian gooseberry), Bela (Bael or wood apple), and Mango. Before collecting the fruits, locals often engage in a ritual of praying to these trees before picking the fruit; a practice that links the trees’ health and divine power to human wellbeing. The belief that typhoid may arise from these trees may perhaps as well be connected to these foraging traditions; showcasing how communities understand illness through their customs and environment.
Evolution of Public Health Service in the District
Chandrapur’s public health history has been significantly shaped by its environmental conditions. The district’s climate, characterized by specific humidity, rainfall, and temperature patterns, has created conditions conducive to various infectious diseases, as documented in the district gazetteer. Over the years, organized public health efforts have played a key role in reducing the fatality rates of these diseases.
Disease Control Initiatives: 1948-1958
The post-independence period saw systematic efforts to address prevalent diseases in Chandrapur. In January 1948, authorities established three Malaria Control Units across the district talukas in response to malaria cases, which were reportedly linked to environmental conditions. A decade later, in 1958, the establishment of a National Filaria Control Unit addressed the growing presence of filariasis in the region. During this same period, the district faced smallpox outbreaks in 1957 and 1958, leading to extensive vaccination campaigns.
Contemporary Challenges: Water Management & Healthcare Accessibility
More recently, the region has contended with cholera outbreaks, with the most recent cases reported in 2022. The ongoing challenge of providing safe drinking water has been identified as a critical factor contributing to these outbreaks.
Notably, the State Water Plan’s Minutes of Meeting (MoM) in 2019 illuminates that there are many critical water quality and management issues which need to be addressed in the district. It is noted in the report that, when conducting a study to frame their basin plans, the officials found that “the east Vidarbha region,” where this district falls, “clearly indicate that in most cases the quality of water provided for domestic purposes is not being systematically tested as per the CPHEEO [Central Public Health and Environmental Engineering Organisation] norms.” Furthermore, it has been highlighted in the report “that the water [here] is not potable as it contains unacceptable levels of bacterial contamination.” The reports and the outbreaks of cholera, hence, in many ways, underscore the need for continued public health interventions when it comes to sanitation and water quality in the region.
COVID-19 in Chandrapur
Among the many concerns that the State Water Plan’s MOM (2019) brought to light is that in Maharashtra, there are a few districts, with Chandrapur being one, where “villages are not connected with any Public Health Centres (PHCs) or Hospitals for several months during each year.” This anecdote about accessibility, in many ways, paints a troubling picture of the everyday realities of villagers and it also sheds light on the healthcare challenges that are prevalent in the district.
This existing infrastructure challenge became more pronounced during the COVID-19 pandemic. However, this crisis also revealed the crucial role of local individual healthcare workers who have worked at the grassroots level to bridge these infrastructure gaps.
Dr. Ramchandra Danekar
Dr. Ramchandra Danekar is a homeopathic doctor, who has for nearly 60 years, provided mobile medical services to Chandrapur’s underserved rural communities. His commitment to rural healthcare emerged early in his career when, years after completing his Diploma and briefly working as a lecturer in the city, he chose instead to serve in regions which have limited healthcare access. Dr. Danekar began his practice in rural Chandrapur through a simple yet unique approach. He, notably, travelled 10-15 kilometers daily by bicycle to deliver door-to-door medical care to residents of remote areas in the district.
The geographical context of Chandrapur, in many ways, shaped Danekar’s distinctive approach to healthcare delivery. “Chandrapur is a remote and highly dense forest area, with many localities where a bus cannot go. Therefore, bicycle or walking are the only options to reach the faraway hamlets and treat the people,” Danekar explained in an interview with New Indian Express (2020).
During the COVID-19 pandemic, when healthcare access became particularly challenging in remote areas, Danekar maintained his daily medical rounds. “In the pandemic times, too, many people could not afford to go to hospitals. So, I decided to treat them at home,” he said. His continued service during this period provided essential medical access to communities already facing significant healthcare infrastructure limitations.
Graphs
Healthcare Facilities and Services
Morbidity and Mortality
Maternal and Newborn Health
Family Planning
Immunization
Nutrition
Sources
Alex George, Sunil Nandraj. 1993. State of Health Care in Maharashtra: A Comparative Analysis
Anuradha Mascarenhas. 2022. "Maharashtra Reports 25 Outbreaks of Cholera." The Indian Express.https://indianexpress.com/article/cities/pun…
George, Mathew. 2023. "The Real Purpose of the Medical College." The Hindu. Accessed March 18, 2025.https://www.thehindu.com/opinion/op-ed/the-r…
Government Medical College, Chandrapur. "Courses Offered." GMC Chandrapur.
Government Medical College, Chandrapur." About the Institution." GMC Chandrapur.https://gmcchandrapur.org/About_Institution.…
Indian Council of Medical Research (ICMR). "About Us." ICMR-CRMCH.https://icmr-crmch.org/aboutus.php
Indian Public Health Standards (IPHS). 2012 (revised).Guidelines for District Hospitals (101 to 500 Bedded). Directorate General of Health Services, Ministry of Health & Family Welfare, Government of India.https://nhm.gov.in/images/pdf/guidelines/iph…
M Choksi, B. Patil et al. 2016.Health systems in India.Vol 36 (Suppl 3).Journal of Perinatology.https://pmc.ncbi.nlm.nih.gov/articles/PMC514…
Maharashtra State Gazetteers. 1972. Chandrapur District Gazetteer. Directorate of Government Printing, Stationery & Publications, Government of Maharashtra, Mumbai.
Mesfin H Kahissay, Teferi G Fenta, Heather Boon. 2017."Beliefs and perception of ill-health causation: a socio-cultural qualitative study in rural North-Eastern Ethiopia." BMC Public Health.https://pmc.ncbi.nlm.nih.gov/articles/PMC526…
New Indian Express. 2020. "60 Years of Selfless Service by 87-Year-Old Homeopathy Doctor in Maharashtra." The New Indian Express.https://www.newindianexpress.com/good-news/2…
S. Khan. 2006. "Systems of Medicine and Nationalist Discourse in India: Towards 'New Horizons' in Medical Anthropology and History. Vol. 62. No. 11. Social Science & Medicine.https://www.sciencedirect.com/science/articl…
Sangeeta Ojha. 2020. "87-Year-Old Doctor Braves COVID-19 Pandemic to Treat Villagers in Maharashtra." Mint.https://www.livemint.com/news/india/87-year-…
Sujata Sinha, Tulika Seth, Roshan B Colah, Alan H Bittles. 2019. "Haemoglobinopathies in India: estimates of blood requirements and treatment costs for the decade 2017–2026." Vol 11, no 1. Journal of Community Genetics ..https://pmc.ncbi.nlm.nih.gov/articles/PMC696…
Syal Kumar, Gustav J Dobos,Thomas Rampp. 2016. "The Significance of Ayurvedic Medicinal Plants." Vol. 22, No. 3. Journal of Evidence-Based Complementary & Alternative Medicine.https://pubmed.ncbi.nlm.nih.gov/?term=%22Kum…
Tutri Ventures. 2024.The Biggest Government Hospital in the village of Pomburna in Chandrapur, Maharashtra.YouTube.https://www.youtube.com/watch?v=PdvvVEOk3sc
Vol. 28, No. 32/33. Economic and Political Weekly.https://www.jstor.org/stable/4400025?seq=1
Water Resources Department, Government of Maharashtra. 2019. Integrated State Water Plan: Volume I. Water Resources Department, Maharashtra.https://wrd.maharashtra.gov.in/Site/Upload/P…
Water Resources Department. 2019. Integrated State Water Plan: Volume I, Minutes of 6th Meeting dated 11/02/2019 (Forming part of ISWP). Water Resources Department, Maharashtra.https://wrd.maharashtra.gov.in/Site/Upload/P…
World Health Organization (WHO). "Typhoid." World Health Organization.https://www.who.int/news-room/fact-sheets/de…
Last updated on 6 November 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.