Contents
- Healthcare Infrastructure
- The Three-Tiered Structure of the District
- Medical Education & Research
- Grant Medical College
- Medical Researchers & Scientists
- Sir Temulji Bhicaji Nariman
- Rukhmabai
- Rani Lakshmibai Rajwade
- Dr. Banoo Jehangir Coyaji
- Dr. Kamal Jayasing Ranadive
- Dr. Indira Hinduja
- Dr. Nandita Patil Palshetkar
- Dr. Alaka Keshav Deshpande
- NGOs & Initiatives
- The Evolution of Public Health Services in the District
- Early Plague Outbreaks
- The 1896 Bubonic Plague
- Dharavi Model
- The Migrant Crisis
- Sanitation | Public Toilets & Cleanliness
- Graphs
- Healthcare Facilities and Services
- A. Public and Govt-Aided Medical Facilities
- B. Private Healthcare Facilities
- C. Approved vs Working Anganwadi
- D. Anganwadi Building Types
- E. Anganwadi Workers
- F. Patients in In-Patients Department
- G. Patients in Outpatients Department
- H. Outpatient-to-Inpatient Ratio
- I. Patients Treated in Public Facilities
- J. Operations Conducted
- K. Hysterectomies Performed
- L. Share of Households with Access to Health Amenities
- Morbidity and Mortality
- A. Reported Deaths
- B. Cause of Death
- C. Reported Child and Infant Deaths
- D. Reported Infant Deaths
- E. Select Causes of Infant Death
- F. Number of Children Diseased
- G. Population with High Blood Sugar
- H. Population with Very High Blood Sugar
- I. Population with Mildly Elevated Blood Pressure
- J. Population with Moderately or Severely High Hypertension
- K. Women Examined for Cancer
- L. Alcohol and Tobacco Consumption
- Maternal and Newborn Health
- A. Reported Deliveries
- B. Institutional Births: Public vs Private
- C. Home Births: Skilled vs Non-Skilled Attendants
- D. Live Birth Rate
- E. Still Birth Rate
- F. Maternal Deaths
- G. Registered Births
- H. C-section Deliveries: Public vs Private
- I. Institutional Deliveries through C-Section
- J. Deliveries through C-Section: Public vs Private Facilities
- K. Reported Abortions
- L. Medical Terminations of Pregnancy: Public vs Private
- M. MTPs in Public Institutions before and after 12 Weeks
- N. Average Out of Pocket Expenditure per Delivery in Public Health Facilities
- O. Registrations for Antenatal Care
- P. Antenatal Care Registrations Done in First Trimester
- Q. Iron Folic Acid Consumption Among Pregnant Women
- R. Access to Postnatal Care from Health Personnel Within 2 Days of Delivery
- S. Children Breastfed within One Hour of Birth
- T. Children (6-23 months) Receiving an Adequate Diet
- U. Sex Ratio at Birth
- V. Births Registered with Civil Authority
- W. Institutional Deliveries through C-section
- X. C-section Deliveries: Public vs Private
- Family Planning
- A. Population Using Family Planning Methods
- B. Usage Rate of Select Family Planning Methods
- C. Sterilizations Conducted (Public vs Private Facilities)
- D. Vasectomies
- E. Tubectomies
- F. Contraceptives Distributed
- G. IUD Insertions: Public vs Private
- H. Female Sterilization Rate
- I. Women’s Unmet Need for Family Planning
- J. Fertile Couples in Family Welfare Programs
- K. Family Welfare Centers
- L. Progress of Family Welfare Programs
- Immunization
- A. Vaccinations under the Maternal and Childcare Program
- B. Infants Given the Oral Polio Vaccine
- C. Infants Given the Bacillus Calmette Guerin (BCG) Vaccine
- D. Infants Given Hepatitis Vaccine (Birth Dose)
- E. Infants Given the Pentavalent Vaccines
- F. Infants Given the Measles or Measles Rubella Vaccines
- G. Infants Given the Rotavirus Vaccines
- H. Fully Immunized Children
- I. Adverse Effects of Immunization
- J. Percentage of Children Fully Immunized
- K. Vaccination Rate (Children Aged 12 to 23 months)
- L. Children Primarily Vaccinated in (Public vs Private Health Facilities)
- Nutrition
- A. Children with Nutritional Deficits or Excess
- B. Population Overweight or Obese
- C. Population with Low BMI
- D. Prevalence of Anaemia
- E. Moderately Anaemic Women
- F. Women with Severe Anaemia being Treated at an Institution
- G. Malnourishment Among Infants in Anganwadis
- Sources
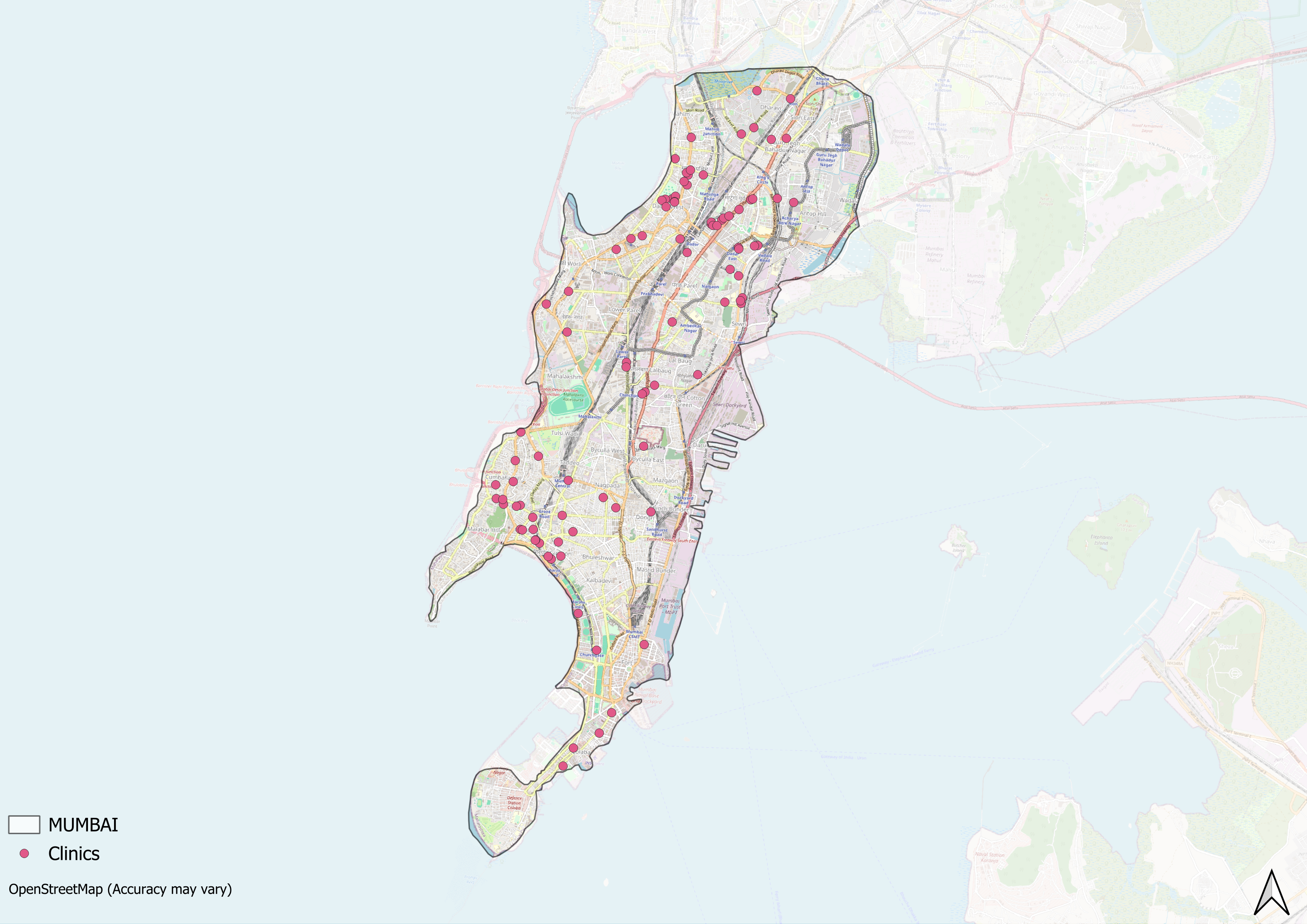
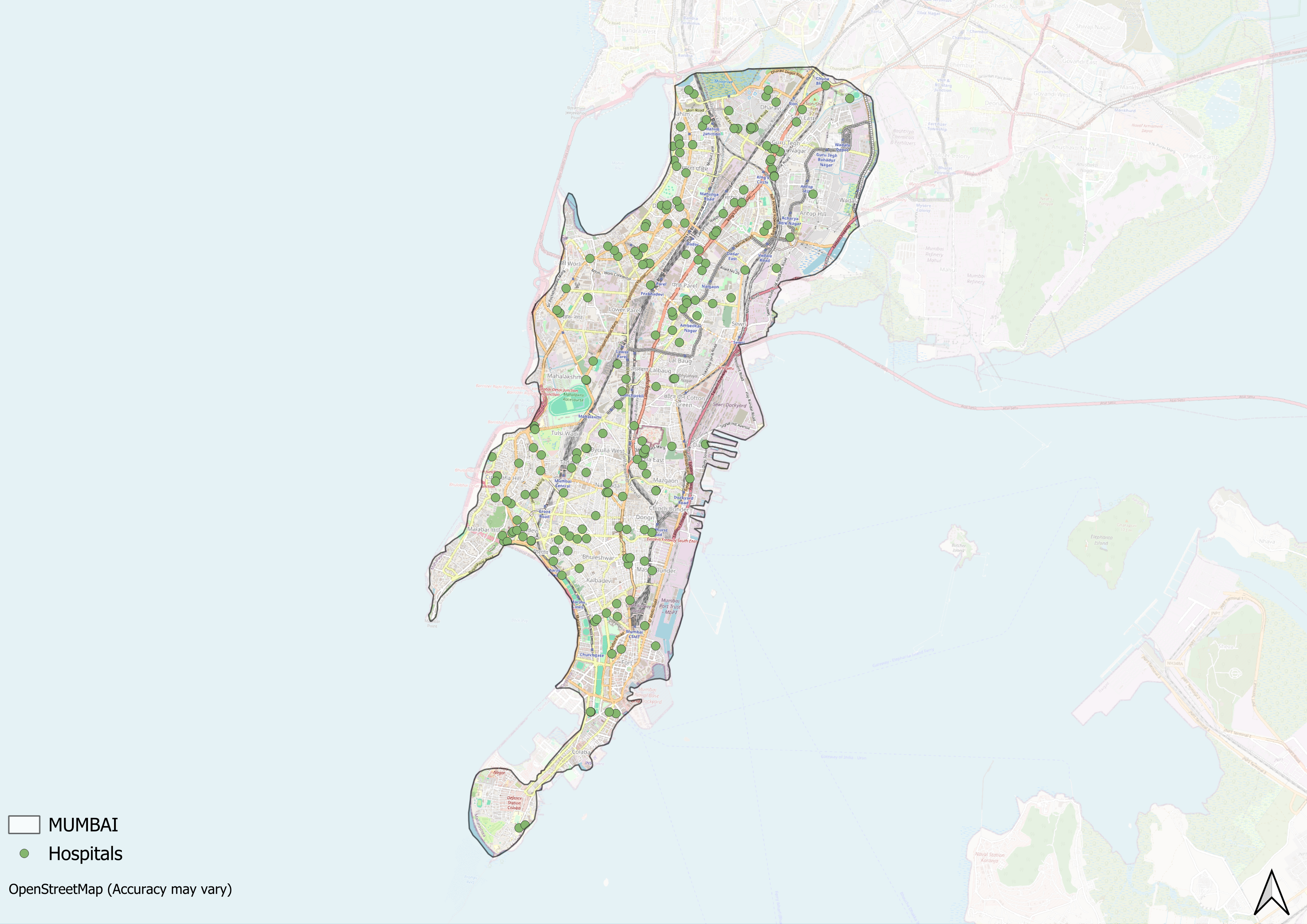
MUMBAI
Health
Last updated on 26 July 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.
Mumbai City’s healthcare landscape, like many other regions across India, is shaped by a mix of indigenous and Western medical practices. For centuries, indigenous knowledge and treatments provided by practitioners such as hakims and vaidyas have formed the foundation of healthcare in the region. The foundations of Mumbai’s modern healthcare infrastructure began to take clearer form during the British colonial period, when the city — then known as Bombay — emerged as a prominent port and commercial center.
Early developments included hospitals like St. George’s, which dates back to the late 17th century under Governor Gerald Aungier’s administration. The 19th century saw further milestones with the establishment of Sir J.J. Hospital and Grant Medical College, laying important groundwork for public health services and medical education not only in Mumbai but across the wider region. Over the decades, Mumbai has continued to evolve as a hub for medical care, research, and education. The city is home to renowned institutions such as Tata Memorial Hospital, recognized for its contributions to cancer treatment and research, and innovators like Dr. Mukesh Batra, who played a key role in expanding modern homeopathy in India. Many leading medical figures and institutions based in Mumbai have also continued to shape advances in healthcare delivery, education, and research across India.
Healthcare Infrastructure
Mumbai City’s healthcare infrastructure aligns with the broader Indian model, which is characterized by a multi-tiered system comprising both public and private sectors. Currently, the public healthcare system is tiered into primary, secondary, and tertiary levels. Primary care is provided through Sub Centres and Primary Health Centres (PHCs), while secondary care is managed by Community Health Centres (CHCs) and Sub-District hospitals. Tertiary care, the highest level, includes Medical Colleges and District Hospitals. This system has been shaped and refined over time, influenced by national healthcare reforms.
The Three-Tiered Structure of the District
The beginnings of organised healthcare in Mumbai can be traced to the 17th century, when formal medical care took root under early colonial administration. According to the colonial district Gazetteer (1909), Gerald Aungier, then Governor of Bombay, supported the creation of a hospital in 1675 to serve military personnel and civilians alike.
By 1677, this early facility was operating from an old court building and continued until the early 1700s, when it was shifted near the Marine Yard. This hospital later formed the basis for what became St. George’s Hospital, which opened in 1889 and continues to function as one of the city’s major public hospitals.
As Bombay, as the district was then called, expanded into a major commercial hub under British rule, new hospitals and dispensaries emerged to serve its growing population. The 19th century, very notably, saw the rise of private dispensaries and multispecialty hospitals that provided care to merchants, workers, and traders drawn to the city (it is important to note that these efforts were very early and progressive for its time).
In 1845, Sir J.J. Hospital was founded in Byculla through the philanthropy of Sir Jamsetjee Jeejeebhoy, whose donation supported the development of one of the city’s earliest major government hospitals. The Grant Medical College, which remains attached to the hospital, continues to train medical professionals to this day.
![An archival image of JJ Hospital, Mumbai City[1]](/media/statistic/images/maharashtra/mumbai/health/an-archival-image-of-jj-hospital-mumbai-city1_sEvGfcy.jpg)
In the early 20th century, Mumbai’s healthcare services expanded further. In 1906, Dr. A.M. Masina established Masina Hospital using a building that had once been the residence of David Sassoon, a noted businessman and philanthropist who contributed to various public welfare projects in western India (he notably also had a hospital in Pune that was named after him). The hospital remains a charitable trust-run facility offering accessible care in central Mumbai.
![The Main building of the Masina Hospital, which used to be the palatial residence of David Sassoon[2]](/media/statistic/images/maharashtra/mumbai/health/the-main-building-of-the-masina-hospital-whic_P8dJfoq.jpg)
Healthcare services gradually expanded beyond the island city into neighbouring areas as new neighbourhoods emerged. In 1947, the Lokmanya Tilak Municipal General Hospital, more commonly known as Sion Hospital, was established near the city’s then northern limits. The hospital was built to serve both the urban population and growing settlements in adjoining suburban zones. Sion Hospital continues to be one of Mumbai’s busiest multispecialty hospitals under the Brihanmumbai Municipal Corporation (BMC).
Specialised care facilities also took shape during the mid-20th century. In 1941, the Sir Dorabji Tata Trust established Tata Memorial Hospital in Parel, which, remarkably, became India’s first dedicated centre for cancer treatment and research. The hospital brought together cancer diagnosis, treatment, and palliative care, contributing to national advances in oncology and serving patients from across India and neighbouring countries.
![Tata Memorial Hospital[3]](/media/statistic/images/maharashtra/mumbai/health/tata-memorial-hospital3-c8e0e1e6.png)
In addition to major public hospitals and large private centres, Mumbai has seen continued growth in homeopathy clinics and traditional treatment centres over the last few decades. In 1982, Dr. Mukesh Batra opened a small homeopathy clinic that introduced computerised systems for treatment and record-keeping. Over time, this clinic expanded into a network of homeopathy centres across India, offering consultations as well as wellness products related to haircare, skincare, and daily health needs.
Medical Education & Research
Medical education and research are foundational to a district's healthcare infrastructure. As Mathew Gerge aptly highlights, medical institutions often serve a “dual purpose,” which includes educating future healthcare professionals and providing healthcare services to the local population. The medical education landscape in Mumbai City spans multiple healthcare traditions such as allopathy, ayurveda, and homeopathy, which is something that captures India’s pluralistic healthcare traditions. It, most significantly, also emerged as the one of the earliest centres for medical education and research in the entire State.
Grant Medical College
Named after Sir Robert Grant, the then Governor of Bombay, Grant Medical College was one of the earliest medical institutions in India, which was built to advance healthcare and formal medical training.

Over the decades, Grant Medical College became an important centre for medical research and training. Notable scientific work conducted there includes V. M. Haffkine’s development of the plague vaccine in 1896 at the F.D. Petit Laboratory (today’s pharmacology lecture hall). In 1902, renowned German microbiologist Robert Koch also carried out research on Vibrio cholerae in the college premises. It is, notably, regarded by many to be a significant hub for biomedical research in India.
Medical Researchers & Scientists
Alongside educational institutions, Mumbai City is also home to many researchers and medical scientists who have carved out their name in medical research and public health services.
Sir Temulji Bhicaji Nariman
Sir Temulji Bhicaji Nariman, born on 3 September, 1848, in Navsari, Gujarat, was a pioneering Indian physician and public health reformer. He studied medicine at Grant Medical College in Mumbai and became the first graduate of the University of Mumbai (then Bombay) to serve as its medical dean after earning his licentiate in 1872. His medical career was marked by dedication to both clinical care and systemic healthcare improvements.
![Sir Temulji Bhicaji Nariman[4]](/media/statistic/images/maharashtra/mumbai/health/sir-temulji-bhicaji-nariman4-e3fa1d47.png)
One of his most notable achievements was the founding of the Parsi Lying-in Hospital in Mumbai, which opened in 1895. Deeply concerned about the high rates of maternal mortality due to puerperal fever, Nariman helped establish this institution to provide safe and hygienic maternity care. Under his leadership for over two decades, the hospital became a model for obstetric care.
His contributions to medicine and public health were widely recognized. He was awarded the Kaisar-i-Hind Medal in 1909 for his public service and was knighted in 1914 in recognition of his exceptional work during the plague epidemic in India. He also held prominent positions such as vice president and president of the College of Physicians and Surgeons of Bombay.
In addition to his clinical work, he was highly active in civic life. He served as Sheriff of Bombay from 1922 to 1923 and became the first Indian Grand Master of Freemasonry in India, a role he held from 1932 to 1938. He was also admitted as a Fellow of the Royal College of Surgeons of Edinburgh in 1922 and is said to have assisted in over 25,000 maternity cases throughout his career. Although the Parsi Lying-in Hospital closed in the 1960s, the building still stands as a lasting tribute to his commitment to maternal health and medical advancement in India.
Rukhmabai
Rukhmabai (22 November 1864 – 25 September 1955) was an Indian physician and an early advocate for women’s rights whose legal battle against child marriage became widely known in the late 19th century. She is recognised as one of the first Indian women to practise Western medicine during the colonial period.
![Rukhmabai[5]](/media/statistic/images/maharashtra/mumbai/health/rukhmabai5-9fcb4214.png)
Born in Mumbai, Rukhmabai was married off at a young age but refused to live with her husband which led to a lengthy court battle between 1884 and 1888. The case drew widespread attention in India and Britain, raising questions about personal freedom, consent, and social reform at a time when legal protections for women were limited. Her defiance and the public discussions that followed contributed to the passage of the Age of Consent Act in 1891, which increased the legal age of consent for girls.
Supporters from India and abroad rallied behind her decision to continue her education. With help from reformers like Shivajirao Holkar and British suffragists including Eva McLaren and Walter McLaren, funds were raised through the “Rukhmabai Defence Committee.” In 1889, she sailed to England to study medicine. She earned her degree from the London School of Medicine for Women in 1894 and trained further at the Royal Free Hospital. Unlike some of her pioneering contemporaries, she returned to India to practise, becoming one of the few Indian women doctors at the time.
Rukhmabai worked first as Chief Medical Officer at the Women’s Hospital in Surat and later at the Zenana State Hospital in Rajkot, where she served until her retirement in 1929. During her career, she also helped found a local branch of the Red Cross Society and remained active in public health initiatives. After retiring, she settled in Gamdevi (which lies in Mumbai City), where she lived until her death.
Rani Lakshmibai Rajwade
Rani Lakshmibai Rajwade (born Lakshmi Joshi, c. 1887–1984) was an Indian physician and an early advocate for women’s rights, family planning, and political representation. She was the daughter of Sir Moropant Vishvanath Joshi, a lawyer and political figure, and Lady Yashodabai Joshi. She studied medicine at Grant Medical College in Bombay and later continued her medical training in England with the support of Gopal Krishna Gokhale. After marrying Major General C. R. Rajwade, the former ruler of Gwalior, she became known by the title “Rani.”
![Dr. Banoo Jehangir Coyaji[7]](/media/statistic/images/maharashtra/mumbai/health/dr-banoo-jehangir-coyaji7-11ebe7d5.png)
Rani Lakshmibai Rajwade[6]
Throughout her life, she practiced medicine in Mumbai while actively advocating for women’s rights and political representation. She was part of the early suffragist movement in India and, in 1917, joined Sarojini Naidu and Annie Besant in presenting a petition to the Viceroy for women’s representation in legislative councils. Her advocacy extended beyond the vote to broader social reforms for women.
She played a vital role in the All India Women’s Conference, initially serving on the central drafting committee in 1931, then becoming Honorary Secretary in 1935, and President in 1939–1940. A vocal proponent of family planning, she introduced resolutions that called for medically supervised public education on birth control and the need for smaller families, leading to the organization’s formal adoption of a family planning resolution in 1933.
In 1938, she chaired the Subcommittee on Women for the Indian National Congress’s National Planning Committee. Her 1940 report emphasized the importance of reproductive health and acknowledged the economic value of women’s unpaid labor in the home; ideas that were remarkably progressive for their time. She also strongly opposed communalism and promoted secularism and women's empowerment.
On the international stage, Rajwade represented India at sessions of the United Nations Economic and Social Council in 1950 and worked to connect Indian women’s organisations with global networks. She continued to support initiatives focused on women’s empowerment and public health throughout her life. She died in 1984, remembered for her contributions to healthcare, social reform, and the advancement of women’s rights in India.
Dr. Banoo Jehangir Coyaji
Dr. Banoo Jehangir Coyaji (7 September 1917 – 15 July 2004) was an Indian physician and public health advocate known for her contributions to maternal and child health and rural healthcare in Maharashtra. Born in Mumbai into a Parsi family, she completed her M.D. at Grant Medical College in 1940 and trained as a gynecologist. In 1944, she joined King Edward Memorial (KEM) Hospital in Pune as Chief Medical Officer, where she led the institution for over five decades. During her tenure, she oversaw its growth from a 40-bed maternity unit to a 550-bed teaching hospital and research centre affiliated with B.J. Medical College.
![Dr. Banoo Jehangir Coyaji[7]](/media/statistic/images/maharashtra/mumbai/health/dr-banoo-jehangir-coyaji7-11645884.png)
Concerned about unequal access to healthcare between cities and villages, Dr. Coyaji launched the Vadu Rural Health Project in 1972, which established a primary health centre serving multiple villages near Pune. Building on this, she started a community health programme in 1977 that trained around 600 local women in hygiene, nutrition, family planning, and basic healthcare, helping to lower infant mortality rates and improve rural health outcomes.
In 1988, she founded the Young Women’s Health and Development Project to address gaps in education and livelihood opportunities for rural women. The initiative provided training in literacy, embroidery, health awareness, and gender rights, encouraging young women to take active roles in their communities.
Dr. Coyaji also served as an advisor to national and international bodies, including the Government of India, the World Health Organization (WHO), UNFPA, the World Bank, and the Ford Foundation, contributing to policies on family planning, population health, and maternal-child services. Under her leadership, KEM Hospital pioneered one of Maharashtra’s first Medical Social Work departments, began providing non-discriminatory care to HIV patients, and developed programmes that became national references for child development and rural healthcare.
For her contributions, she was honoured with the Padma Bhushan in 1989, the Ramon Magsaysay Award for Public Service in 1993, and the Punyabhushan Award in 1992. Dr. Coyaji’s work remains influential in the fields of community health and women’s empowerment across India.
Dr. Kamal Jayasing Ranadive
Dr. Kamal Jayasing Ranadive was born on 8 November, 1917, in Pune, India. A brilliant student, she pursued Botany and Zoology at Fergusson College and went on to complete a master’s degree in cytogenetics in 1943, followed by a Ph.D. in cytology from Bombay University in 1949. She later undertook postdoctoral research in tissue culture at Johns Hopkins University under George Gey, gaining experience that would greatly influence her pioneering work upon returning to India.
![Dr. Kamal Jayasing Ranadive[8]](/media/statistic/images/maharashtra/mumbai/health/dr-kamal-jayasing-ranadive8-b7e1b634.png)
Ranadive played a crucial role in advancing cancer research in India. She established the country’s first tissue culture laboratory at the Indian Cancer Research Centre (ICRC) in Mumbai, which she later directed. Her innovative work led to the development of animal models for studying various types of cancer, including leukemia and cancers of the breast and esophagus. These models were instrumental in exploring how genetic predisposition, hormones, and viruses influence tumor growth, laying the groundwork for cancer biology in India.
In addition to her cancer research, Dr. Ranadive made significant contributions to the fight against leprosy. She studied Mycobacterium leprae, the bacteria responsible for the disease, helping to advance efforts in vaccine development and treatment strategies. Her research bridged laboratory science with real-world applications, directly impacting public health outcomes.
Even after retiring in 1989, Ranadive remained deeply engaged in community health. She worked extensively in rural Maharashtra, training women as healthcare workers and promoting nutrition, hygiene, and medical awareness among Scheduled Tribe (ST) populations. She also co-founded the Indian Women Scientists' Association (IWSA) in 1973, an organization dedicated to supporting women in scientific careers through childcare services, scholarships, and advocacy.
Throughout her career, Dr. Ranadive published over 200 scientific papers and earned numerous honors, including the Padma Bhushan in 1982. Her work continues to influence public health, medical research, and the role of women in science, making her one of the most impactful biomedical scientists in Indian history.
Dr. Indira Hinduja
Dr. Indira Hinduja (born 21 August 1946) is an Indian gynecologist and fertility specialist known for her pioneering work in helping couples have children through assisted reproduction. She was born in Shikarpur, which was then part of British India, and studied medicine at University of Mumbai, where she completed her MBBS, MD, and PhD. Her main area of research and practice has focused on in vitro fertilisation (IVF) and embryo transfer.
![Dr. Indira Hinduja[9]](/media/statistic/images/maharashtra/mumbai/health/dr-indira-hinduja9-b442e7ff.png)
In August 1986, Dr. Hinduja helped deliver India’s first baby born through IVF — commonly known as the country’s first “test-tube baby” — at King Edward Memorial Hospital in Mumbai. This achievement opened up new possibilities for families facing infertility. She went on to perform India’s first successful Gamete Intra-Fallopian Transfer (GIFT) procedure in 1988 and, in 1991, delivered the country’s first baby conceived with an egg donation.
Throughout her career, Dr. Hinduja has helped more than 15,000 couples become parents through different fertility treatments. She has also introduced new techniques in India, such as screening embryos for genetic conditions before implantation, freezing eggs and embryos for later use, and using advanced methods for selecting healthy sperm. Her work helped make IVF more accepted and accessible in India — a fact reflected in the story of the country’s first test-tube baby, who went on to have her own child years later.
For her contributions, Dr. Hinduja has received many honours, including the Dhanvantari Award, a Lifetime Achievement Award from the Federation of Obstetric and Gynaecological Societies of India, and the Padma Shri, one of India’s highest civilian awards. She continues to work to make fertility treatments better known and more widely available, including promoting options like egg freezing. Her career combines medical progress with patient care and is widely seen as a milestone in India’s medical history.
Dr. Nandita Patil Palshetkar
Dr. Nandita Patil Palshetkar (born 30 October 1963) is an Indian obstetrician and gynecologist known for her work in the field of assisted reproductive technologies (ART). Born in Mumbai, she completed her MBBS and MD in Obstetrics and Gynecology from Grant Medical College in 1993. She later pursued advanced training in in vitro fertilisation (IVF) and micromanipulation techniques at centres in Ghent, Naples, Melbourne, and Copenhagen.
![Dr. Nandita Patil Palshetkar[10]](/media/statistic/images/maharashtra/mumbai/health/dr-nandita-patil-palshetkar10-e78788ae.png)
Dr. Palshetkar is the founder and medical director of Bloom IVF, a network of fertility centres operating in major Indian cities. Over nearly three decades, she has been associated with the introduction of several technologies in India, including intracytoplasmic sperm injection (ICSI), laser-assisted hatching, spindle view imaging, the use of embryoscope technology, and ovarian tissue freezing. She also helped implement non-invasive preimplantation genetic testing (PGT-A) and expanded treatment options for male infertility through techniques such as micro-TESE, IMSI, and single-sperm vitrification.
It is estimated that Dr. Palshetkar’s clinical work has supported over 25,000 couples in achieving parenthood through assisted reproduction, with cases ranging from IVF for partners with hemiplegia to successful pregnancies in women over 60. She has been involved in efforts to make fertility treatments more affordable and accessible, particularly for underserved communities.
Beyond clinical practice, she has held leadership roles in key professional organisations, including serving as President of the Federation of Obstetric and Gynaecological Societies of India (FOGSI) and the Indian Society for Assisted Reproduction (ISAR). She has launched public health initiatives such as “We for Street,” aimed at women’s empowerment, and the “She’s Ambassador” programme, which trains schoolgirls to promote health awareness in their communities.
Dr. Palshetkar has contributed over 100 publications, written chapters for more than 100 books, edited over 25 volumes, and delivered upwards of 85 keynote lectures. Her work has been recognised with honours such as the Bharat Gaurav Award, the Golden Globe Tigers Award, several lifetime achievement awards from FOGSI, and an Honorary Fellowship from the Royal College of Obstetricians and Gynaecologists in London.
Dr. Alaka Keshav Deshpande
Dr. Alaka Keshav Deshpande is an Indian physician and social worker renowned for her pioneering work with HIV/AIDS patients. Based at JJ Hospital in Mumbai, she launched India’s first dedicated HIV Outpatient Department (OPD) in 1990. Demonstrating exceptional commitment to patient care and public health, she went on to establish and lead the hospital's Anti-Retroviral Therapy (ART) section from 2003 to 2011. Notably, she chose to forgo a salary during this period, underscoring her dedication to the cause. In recognition of her outstanding contributions to medicine and social service, she was awarded the Padma Shri, India’s fourth-highest civilian honor, in 2001.
NGOs & Initiatives
The determinants of health and health outcomes, as the World Health Organization (WHO) elaborates, are not solely shaped by more than just medical factors and healthcare services. The organization uses the term “social determinants of health (SDH)” to refer to the “non-medical factors that influence health outcomes.” These non-medical factors can be sanitation, nutrition, community well-being, or, as the WHO outlines, “income and social protection,” “food security,” access to quality healthcare, and more.
While there have been ongoing efforts to strengthen Mumbai district’s healthcare infrastructure, certain areas still face challenges, particularly in addressing these broader health determinants. In response, non-governmental organizations have emerged as vital partners, working alongside public health systems to develop innovative, grassroots-level approaches that bridge these gaps.
SNEHA
The Society for Nutrition, Education and Health Action (SNEHA) is a Mumbai-based non-governmental organisation founded in 1999 by Dr. Armida Fernandez, a former dean of Lokmanya Tilak Municipal Medical College and Hospital. SNEHA was established to address issues related to the health and nutrition of women and children living in urban informal settlements. Its areas of work include reproductive health, maternal and child nutrition, mental health, and the prevention of gender-based violence.
![SNEHA[11]](/media/statistic/images/maharashtra/mumbai/health/sneha11-9a40e13d.png)
In recent years, SNEHA has partnered with the H.T. Parekh Foundation, the Integrated Child Development Services (ICDS), and the Brihanmumbai Municipal Corporation (BMC) to implement targeted programmes in areas such as Mankhurd, Govandi, and Dharavi. These initiatives have focused on providing nutrition counselling, monitoring child growth, and identifying and referring cases of child malnutrition to appropriate facilities.
Notably, data from the organisation’s programmes indicate a reduction in the prevalence of anaemia among pregnant and lactating women in the targeted areas, decreasing from an estimated 52% in 2021 to 38% in 2024. Improvements in maternal health have been linked to better child health outcomes, including a decrease in rates of stunting, wasting, and underweight among children under five years of age.
The Evolution of Public Health Services in the District
Public health services in Mumbai City have developed over centuries in response to epidemics, urban growth, and changing social needs. Historical accounts show how major disease outbreaks, public resistance, and local initiatives have shaped health infrastructure and community responses over time.
Early Plague Outbreaks
Records indicate that Mumbai experienced one of its earliest severe plague outbreaks between 1690 and 1708. Conditions linked to this epidemic included prolonged flooding, excessive rainfall, and the practice of fertilising coconut palms with rotting fish. These factors created unsanitary environments that contributed to the spread of disease.
The 1896 Bubonic Plague
A major turning point in the city’s public health history occurred with the bubonic plague epidemic that began in 1896. This outbreak was part of a larger wave that originated in China in the mid-19th century and spread to India’s port cities through maritime trade. Initial responses relied heavily on quarantine laws, compulsory isolation, inspections of travellers, and the forced disinfection or demolition of infected houses.
![Burning Clothes of a Suspected Patient during House-to-House Visitations[12]](/media/statistic/images/maharashtra/mumbai/health/burning-clothes-of-a-suspected-patient-during_CjOqOCR.png)
These measures, however, were deeply unpopular and often created fear and unrest among local residents, many of whom left the city in large numbers to avoid forced inspections and isolation. One of the few documented glimpses into how people perceived this medical response comes from the writings of Pandita Ramabai Saraswati. In Pune, Ramabai raised her concerns directly with the then Governor of Bombay, Lord Sandhurst, and wrote a long letter to the editor of the Bombay Guardian criticising how suspected plague patients were treated in government segregation camps.
Her letter attracted significant attention at the time and was even read aloud in the British Parliament. She wrote, “The shameful way in which women were made to submit to treatment by male doctors goes to prove that English authorities in general do not believe that Indian women are honest and need special consideration… How would an English woman, poor though she may be, like to be exposed to the public gaze and roughly handled by male doctors?”
Some significant steps were taken in the field of medicine at the time, including the identification of the plague bacillus and the development of a vaccine by Dr. Waldemar Haffkine in 1897. Yet official efforts were often limited by inexperience and by fears that strict quarantine rules might disrupt port trade. By 1899, the outbreak had largely subsided, but the challenges and public resistance during this period shaped how sanitation and epidemic control would be managed in the years to come.
Dharavi Model
Public health challenges continued to evolve in the 21st century. When COVID-19 reached Mumbai in early 2020, Dharavi—often described as one of the world’s largest informal settlements—was at high risk due to its extreme population density and limited sanitation facilities. Despite these conditions, Dharavi’s response drew international attention for its swift and localised approach. Within days of the first confirmed case, local authorities set up fever clinics and deployed over 2,000 health workers.
The strategy, described as “4Ts” (tracing, tracking, testing, treatment), helped contain the virus. By the time the second wave arrived, Dharavi’s infection growth rate was among the city’s lowest. The World Health Organization recognised Dharavi’s approach as an effective urban public health model for managing outbreaks in dense settlements.
The Migrant Crisis
The pandemic highlighted the risks to public health on both macro and micro levels, demonstrating how large-scale events affect our everyday lives. Movements were stopped in a city characterized by its constant movement and speed.
Industries came to a standstill, and migrants, who were integral to the city’s workforce, struggled as they were forced to walk back to their homes across states and even the country due to a lack of money. This crisis exposed the city's underlying issues with expenses and wages, revealing how unsustainable income levels can become in times of public health and economic hardship. Additionally, it brought forth issues faced by economically weaker sections of society, as their hardships were visibly sidelined during the early stages of the pandemic.
Sanitation | Public Toilets & Cleanliness
Access to clean and safe public toilets has long been an uneven aspect of Mumbai’s urban services. While residents in affluent areas generally have access to maintained facilities, people living in informal settlements or lower-income neighbourhoods often face significant challenges in finding usable public toilets. These disparities are shaped by factors including income, caste, and especially gender.
The ‘Right to Pee’ campaign emerged in Mumbai City in response to this gap. Launched in 2011 by a collective of women’s rights activists, journalists, and urban planners, the movement highlighted how the lack of accessible and hygienic toilets disproportionately affects women and girls in the city.
The campaign’s demands have focused on three main goals: providing free and safe public toilets for women, ensuring adequate maintenance and water supply, and expanding the number of facilities in both urban centres and transport hubs. Activists have argued that access to safe toilets is directly linked to women’s health, safety, mobility, and dignity.
Over nearly a decade, ‘Right to Pee’ has organised public awareness drives, community meetings, and policy dialogues with municipal authorities such as the Brihanmumbai Municipal Corporation (BMC).
Graphs
Healthcare Facilities and Services
Morbidity and Mortality
Maternal and Newborn Health
Family Planning
Immunization
Nutrition
Sources
B. Arunachalam, et al. 1986-87. Maharashtra State Gazetteers: Greater Bombay District. Vol. I, II, III. Gazetteers Department, Govt of Maharashtra. Mumbai.
M Choksi, B. Patil et al. 2016. Health systems in India. Vol 36 (Suppl 3).Journal of Perinatology.https://pmc.ncbi.nlm.nih.gov/articles/PMC514…
Mathew George. 2023. "The Real Purpose of the Medical College." The Hindu.https://www.thehindu.com/opinion/op-ed/the-r…
National Army Museum, UK. "The Bombay Plague." National Army Museum.https://www.nam.ac.uk/explore/bombay-plague
Nioshi Shah. 2020. "Right to Pee: Gender, Caste, and the Privileges of Urination." Feminism in India, India.https://feminisminindia.com/2020/04/10/right…
Preeti Chopra. 2012. Free to move, forced to flee: the formation and dissolution of suburbs in colonial Bombay, 1750–1918. Vol. 39, no. 1. Urban Historyhttps://www.jstor.org/stable/26398118?seq=15
Purnima Sah. 2024. "Anaemia Among Pregnant and Lactating Women Down from 52% to 38% in Mumbai Slums: Survey." The Hindu.https://www.thehindu.com/news/cities/mumbai/…
S. M. Edwardes, et al. 1909. Gazetteer of the Bombay Presidency: Bombay City and Island.Vol. I, II, III. Bombay.
Susie Tharu, and Lalita, eds. 1991. Women Writing in India, Volume I: 600 BC to the Early Twentieth Century.New Delhi: Oxford University Press.
Team YS. 2021. "Dr. Batra: An Accidental Entrepreneur Who Built a Business with Passion and Values." YourStory.https://yourstory.com/2021/07/dr-batra-accid…
Vallabh Rao. 2018. "How Mumbai-Based Non-Profit SNEHA Impacted the Lives of 37,000 Pregnant Women and 25,000 Undernourished Children." YourStory.https://yourstory.com/2018/04/mumbai-based-n…
Wikipedia Contributors. Alka Despamde. Wikipediahttps://en.wikipedia.org/wiki/Alaka_Deshpande
Wikipedia Contributors. Banoo Jehangir Coyaji. Wikipediahttps://en.wikipedia.org/wiki/Banoo_Jehangir…
Wikipedia Contributors. Indira Hinduja. Wikipedia.https://en.wikipedia.org/wiki/Indira_Hinduja
Wikipedia Contributors. Kamal Randive. Wikipedia.orghttps://en.wikipedia.org/wiki/Kamal_Ranadive
Wikipedia Contributors. Lakshmibai Rajwade. Wikipedia.https://en.wikipedia.org/wiki/Lakshmibai_Raj…
Wikipedia Contributors. Nandita P Palshetkar. Wikipediahttps://en.wikipedia.org/wiki/Nandita_P._Pal…
Wikipedia Contributors. Rukhmabai. Wikipedia.https://en.wikipedia.org/wiki/Rukhmabai
Wikipedia Contributors. Temulji Bhicaji Nariman. Wikipedia.https://en.wikipedia.org/wiki/Temulji_Bhicaj…
World Health Organization (WHO). 2025. "Social Determinants of Health." World Health Organization.https://www.who.int/health-topics/social-det…
Last updated on 26 July 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.