Contents
- Healthcare Infrastructure
- Graphs
- Healthcare Facilities and Services
- A. Public and Govt-Aided Medical Facilities
- B. Private Healthcare Facilities
- C. Approved vs Working Anganwadi
- D. Anganwadi Building Types
- E. Anganwadi Workers
- F. Patients in In-Patients Department
- G. Patients in Outpatients Department
- H. Outpatient-to-Inpatient Ratio
- I. Patients Treated in Public Facilities
- J. Operations Conducted
- K. Hysterectomies Performed
- L. Share of Households with Access to Health Amenities
- Morbidity and Mortality
- A. Reported Deaths
- B. Cause of Death
- C. Reported Child and Infant Deaths
- D. Reported Infant Deaths
- E. Select Causes of Infant Death
- F. Number of Children Diseased
- G. Population with High Blood Sugar
- H. Population with Very High Blood Sugar
- I. Population with Mildly Elevated Blood Pressure
- J. Population with Moderately or Severely High Hypertension
- K. Women Examined for Cancer
- L. Alcohol and Tobacco Consumption
- Maternal and Newborn Health
- A. Reported Deliveries
- B. Institutional Births: Public vs Private
- C. Home Births: Skilled vs Non-Skilled Attendants
- D. Live Birth Rate
- E. Still Birth Rate
- F. Maternal Deaths
- G. Registered Births
- H. C-section Deliveries: Public vs Private
- I. Institutional Deliveries through C-Section
- J. Deliveries through C-Section: Public vs Private Facilities
- K. Reported Abortions
- L. Medical Terminations of Pregnancy: Public vs Private
- M. MTPs in Public Institutions before and after 12 Weeks
- N. Average Out of Pocket Expenditure per Delivery in Public Health Facilities
- O. Registrations for Antenatal Care
- P. Antenatal Care Registrations Done in First Trimester
- Q. Iron Folic Acid Consumption Among Pregnant Women
- R. Access to Postnatal Care from Health Personnel Within 2 Days of Delivery
- S. Children Breastfed within One Hour of Birth
- T. Children (6-23 months) Receiving an Adequate Diet
- U. Sex Ratio at Birth
- V. Births Registered with Civil Authority
- W. Institutional Deliveries through C-section
- X. C-section Deliveries: Public vs Private
- Family Planning
- A. Population Using Family Planning Methods
- B. Usage Rate of Select Family Planning Methods
- C. Sterilizations Conducted (Public vs Private Facilities)
- D. Vasectomies
- E. Tubectomies
- F. Contraceptives Distributed
- G. IUD Insertions: Public vs Private
- H. Female Sterilization Rate
- I. Women’s Unmet Need for Family Planning
- J. Fertile Couples in Family Welfare Programs
- K. Family Welfare Centers
- L. Progress of Family Welfare Programs
- Immunization
- A. Vaccinations under the Maternal and Childcare Program
- B. Infants Given the Oral Polio Vaccine
- C. Infants Given the Bacillus Calmette Guerin (BCG) Vaccine
- D. Infants Given Hepatitis Vaccine (Birth Dose)
- E. Infants Given the Pentavalent Vaccines
- F. Infants Given the Measles or Measles Rubella Vaccines
- G. Infants Given the Rotavirus Vaccines
- H. Fully Immunized Children
- I. Adverse Effects of Immunization
- J. Percentage of Children Fully Immunized
- K. Vaccination Rate (Children Aged 12 to 23 months)
- L. Children Primarily Vaccinated in (Public vs Private Health Facilities)
- Nutrition
- A. Children with Nutritional Deficits or Excess
- B. Population Overweight or Obese
- C. Population with Low BMI
- D. Prevalence of Anaemia
- E. Moderately Anaemic Women
- F. Women with Severe Anaemia being Treated at an Institution
- G. Malnourishment Among Infants in Anganwadis
- Sources
SATARA
Health
Last updated on 26 July 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.
Satara’s healthcare landscape, like many other regions across India, is shaped by a mix of indigenous and Western medical practices. For centuries, communities in the district depended on local healers such as hakims and vaidyas, who treated illnesses using plants, herbs, and other resources found in the surrounding forests and fields. This use of local knowledge and natural remedies formed the base of early healthcare in Satara before formal hospitals were established. Over time, these practices continued alongside the introduction and expansion of more specialised medical services.
Healthcare Infrastructure
Similar to other regions in India, Satara’s healthcare infrastructure follows a multi-tiered system that involves both public and private sectors. The public healthcare system is structured into primary, secondary, and tertiary levels. Primary care is provided through Sub Centres and Primary Health Centres (PHCs), secondary care is managed by Community Health Centres (CHCs) and Sub-District hospitals, while tertiary care, the highest level, is delivered through Medical Colleges and District Hospitals.
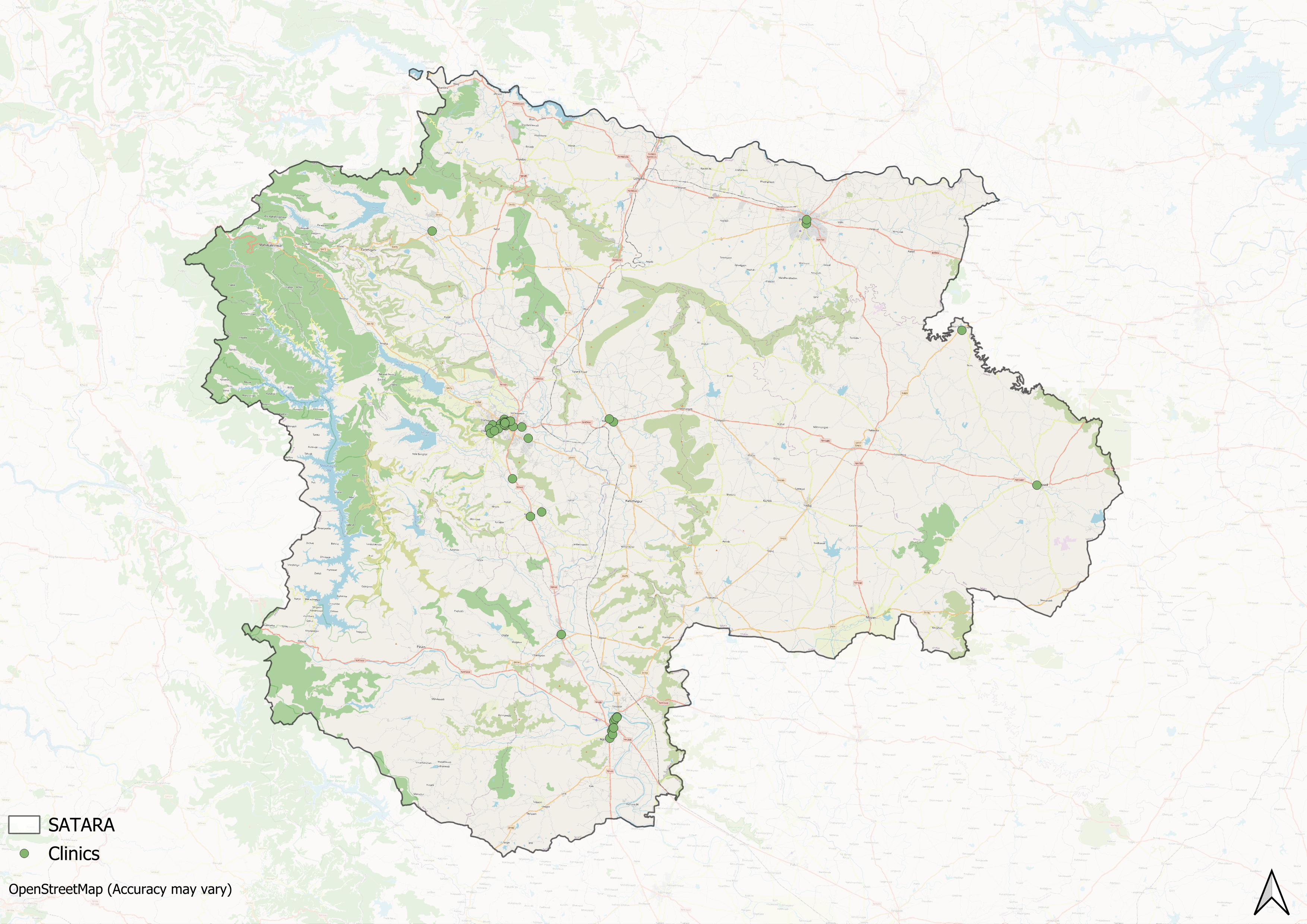
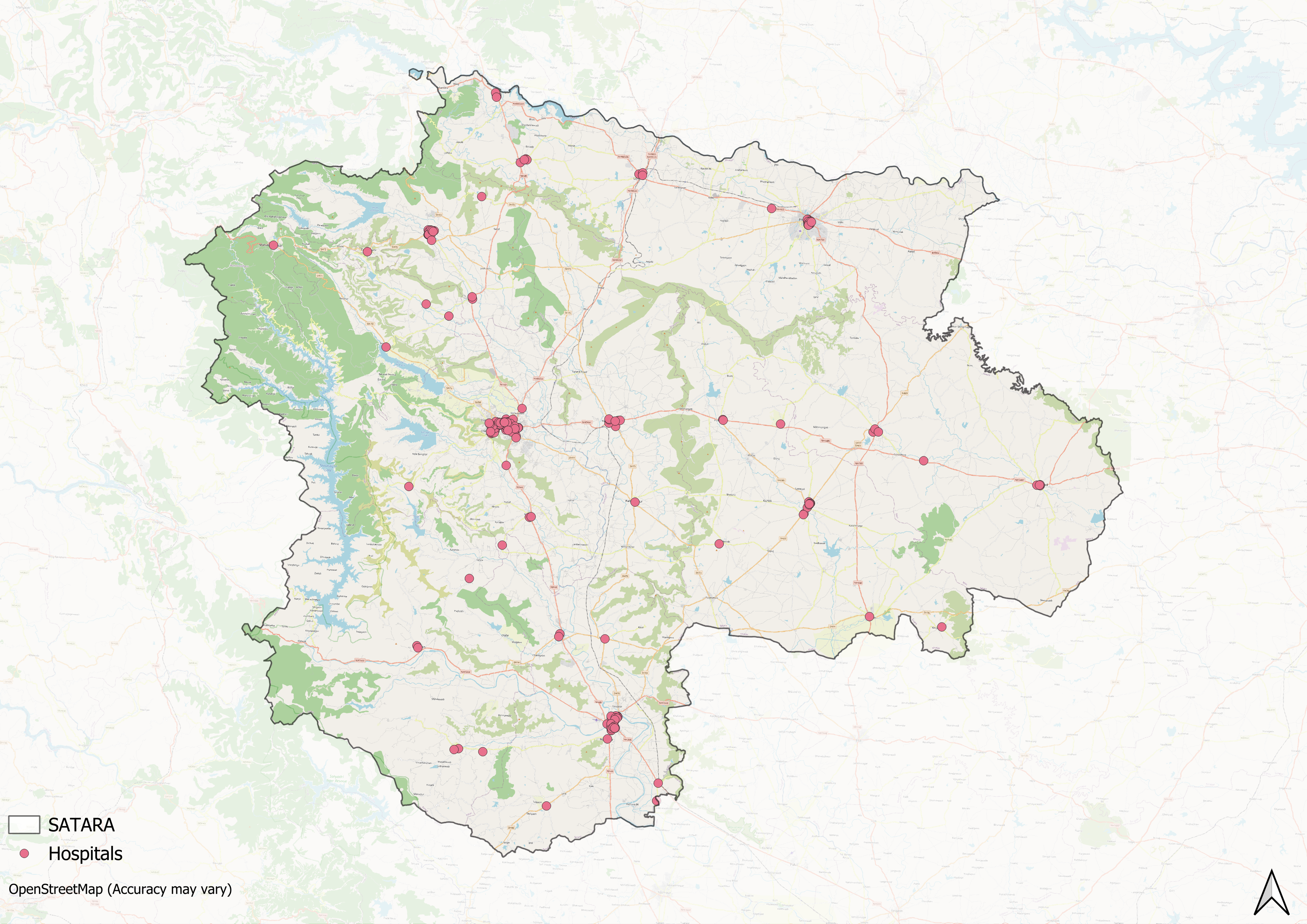
Supporting this structure is a network of Accredited Social Health Activists (ASHAs) who, as described by the National Health Mission, serve as “an interface between the community and the public health system.” Over time, this multi-layered healthcare model has been continuously shaped and refined by national healthcare policies and reforms to improve universal health coverage across regions.
Satara’s formal healthcare infrastructure, like much of India, has its roots in the 19th century. Among the earliest facilities to be built in the region was the Mahabaleshwar Convalescent Hospital, established in 1828. Its founding coincided with Mahabaleshwar’s growth as a British hill station and reflected the need for rest and nursing care for visitors recovering from illness in the cooler hill climate.
Many missionaries and administrative figures contributed to early medical services in Satara. However, as Satara was a princely state during that period, the royal family played a significant role, most notably by establishing one of the district’s largest public healthcare facilities. In 1840, Appa Saheb, the Raja of Satara, laid the foundation for the Satara Civil Hospital.
![Satara Civil Hospital[1]](/media/statistic/images/maharashtra/satara/health/satara-civil-hospital1-816d591f.png)
In the early 20th century, new hospitals were built in the hill region to continue expanding medical services for residents and travellers alike. In Mahabaleshwar, the Morarji Gokaldas Rural Hospital (MGRH) was established in 1914 by Lord Willingdon and named after Seth Morarji Gokaldas, an industrialist from the Bhatia community. Built on 11 acres of forested land, the hospital served both local residents and British visitors but eventually fell into disrepair.
In 2018, the Ministry of Health entrusted its management to the Indian Red Cross Society (IRCS), which also runs the nearby Bel-Air Hospital in Panchgani. Despite challenges such as shortages of medical staff, renewed efforts aim to keep MGRH operating for Mahabaleshwar and surrounding villages.
![Morarji Gokaldas Rural Hospital (MGRH), Mahabaleshwar, Satara district[2]](/media/statistic/images/maharashtra/satara/health/morarji-gokaldas-rural-hospital-mgrh-mahabale_n0oAtZ3.png)
Bel-Air Hospital is another facility which has a notable place in Satara’s medical history. Originally established in Pune in 1912, Bel-Air was moved to Panchgani in 1914 to take advantage of the dry climate, which was considered suitable for tuberculosis care at the time. Its founder, Dr. Rusomji Billimoria, was awarded the first gold medal from the Anti-TB Association of India and the Padma Bhushan in 1961 for his contributions to TB treatment.
![Bel Air Hospital[3]](/media/statistic/images/maharashtra/satara/health/bel-air-hospital3-e70b0c15.png)
Today, Bel-Air functions as a long-term care centre from a campus of 58 heritage bungalows that combine historic architecture with medical services. In 2014, it received the Times of India Healthcare Achievers Award for its work in managing chronic conditions.
Over time, public healthcare facilities in Satara continued to expand beyond these early institutions, while private hospitals and charitable trusts also established new services to meet the district’s growing medical needs.
Graphs
Healthcare Facilities and Services
Morbidity and Mortality
Maternal and Newborn Health
Family Planning
Immunization
Nutrition
Sources
Bel-Air Hospital. "About Us." Bel-Air Hospitalhttps://belairhospital.org/https://belairhospital.org/
FTD Travel. "Mahabaleshwar: A Historical Overview." FTD Travel.https://www.ftd.travel/mahabaleshwar-history
Hemal Ashar. 2020. "A 106-Year-Old Hospital in Mahabaleshwar is Reborn." Mid-Day.https://www.mid-day.com/mumbai/mumbai-news/a…
M Choksi, B. Patil et al. 2016.Health systems in India.Vol 36 (Suppl 3).Journal of Perinatology.https://pmc.ncbi.nlm.nih.gov/articles/PMC514…
Maharashtra State Gazetteers. 1963. Satara District Gazetteer. Gazetteer Department, Government of Maharashtra, Mumbai.
National Health Mission (NHM). "About Accredited Social Health Activist (ASHA)." National Health Mission, India.https://nhm.gov.in/index1.php?lang=1&level=1…
Last updated on 26 July 2025. Help us improve the information on this page by clicking on suggest edits or writing to us.